New FDA-Approved Chronic Pain Treatments in 2025: A Guide

Five cutting-edge treatments for chronic pain have recently received FDA approval in 2025, offering new hope and improved management options for millions of Americans grappling with persistent discomfort, ranging from novel neuromodulation devices to targeted pharmacological therapies.
Living with chronic pain can be a debilitating experience, impacting every facet of one’s life, from daily activities to mental well-being. For years, patients and healthcare providers have sought more effective, less invasive, and safer solutions beyond traditional medications and interventions. The landscape of pain management is continually evolving, driven by scientific innovation and a deeper understanding of pain pathways. As we navigate through 2025, a wave of new medical advancements has emerged, bringing forth promising therapeutic options. This article delves into what are the 5 latest FDA-approved treatments for chronic pain in 2025, exploring their mechanisms, benefits, and how they are set to revolutionize care for those suffering from unrelenting pain.
Understanding Chronic Pain and the Need for New Treatments
Chronic pain, defined as pain lasting longer than three to six months, affects an estimated 50 million adults in the United States. Its pervasive nature makes finding lasting relief a complex challenge. Many existing treatments, while effective for some, often come with significant side effects or limitations, leading to a continuous search for better alternatives. The FDA’s rigorous approval process ensures that new therapies meet stringent safety and efficacy standards before becoming available to the public. These approvals are a testament to years of research and clinical trials, bringing forward solutions designed to offer more targeted relief with fewer adverse effects. The urgent need for innovative treatments stems from the inadequacies of conventional approaches, which can include opioid dependence risks, limited efficacy for neuropathic pain, or invasive surgical procedures with lengthy recovery times. Therefore, the introduction of novel FDA-approved therapies is a beacon of hope for a significant portion of the population.
The economic burden of chronic pain is also immense, costing the nation billions annually in healthcare expenses and lost productivity. Beyond the financial implications, the personal toll on individuals and families is immeasurable. Patients often experience reduced quality of life, depression, anxiety, and social isolation. These statistics underscore the critical importance of developing and approving new treatments that can not only alleviate pain but also restore functionality and overall well-being. The advancements approved in 2025 focus on diverse pain mechanisms, moving beyond a one-size-fits-all approach and offering personalized care tailored to specific types of chronic pain. This shift towards precision medicine in pain management is a significant step forward.
The Evolution of Pain Management
Pain management has come a long way from its early reliance on simple analgesics. Modern approaches incorporate a multidisciplinary strategy, combining pharmacology, physical therapy, psychological support, and interventional procedures. The latest FDA approvals reflect this trend, emphasizing innovation in medical devices and targeted drug delivery. These new treatments are often designed to interfere with pain signals at their source or to modulate the body’s natural pain response systems more effectively. The aim is not just to mask pain, but to address its underlying mechanisms, offering more sustainable and comprehensive relief. This evolution signifies a move towards less systemic and more localized therapies, reducing the overall burden on the patient’s body.
- Advancements in neuromodulation offer device-based solutions that directly influence nerve activity.
- Novel pharmaceuticals target specific pain receptors with greater precision, minimizing off-target effects.
- Biologics and regenerative medicine approaches are exploring the body’s innate healing capabilities.
- Digital therapeutics are emerging as complementary tools for pain management through behavioral changes.
The integration of technology, such as AI and machine learning, is also playing a crucial role in identifying new therapeutic targets and optimizing treatment protocols. This synergy between advanced science and technology is accelerating the pace of discovery and bringing sophisticated solutions to the forefront of chronic pain care. The approvals in 2025 demonstrate a commitment to pushing the boundaries of what is possible in pain relief.
1. Targeted Spinal Cord Stimulation (SCS) with Enhanced AI-Driven Programming
Spinal Cord Stimulation (SCS) has been a cornerstone of neuromodulation for chronic pain for decades, but the latest FDA approval in 2025 introduces a significant leap forward: Targeted SCS with Enhanced AI-Driven Programming. This next-generation device utilizes artificial intelligence to learn and adapt to a patient’s unique pain profile, delivering more precise and personalized electrical impulses to the spinal cord. Unlike previous SCS systems that required extensive manual programming and often resulted in suboptimal pain relief for some, this new system can continuously monitor pain levels and activity patterns, adjusting stimulation parameters in real-time. This dynamic approach leads to more consistent pain relief and a reduction in programming-related visits.
The AI component analyzes vast amounts of patient data to identify optimal stimulation settings, reducing the trial-and-error often associated with conventional SCS. This technology is particularly beneficial for complex regional pain syndrome (CRPS) and failed back surgery syndrome (FBSS), conditions where precise neuromodulation can make a substantial difference. Patients can experience fewer “breakthrough” pain episodes, improved sleep, and a greater ability to engage in daily activities. The device is also designed to be smaller and more discreet, improving patient comfort and adherence. Clinical trials revealed a notable improvement in pain scores and quality of life compared to earlier SCS technologies, marking a new era in implantable pain therapies. The personalized aspect of this treatment addresses the inherent variability of chronic pain presentation.
How AI Transforms SCS Therapy
The integration of AI in SCS technology is revolutionary. Instead of relying on pre-programmed algorithms or doctor-adjusted settings, the AI-driven system uses machine learning to interpret biosignals and patient feedback. This allows for a closed-loop system where the device constantly optimizes its output based on the body’s response. For instance, if a patient is experiencing increased pain during a specific activity, the AI can instantly modify the stimulation pattern to counteract it, providing seamless and adaptive pain relief. This level of responsiveness was previously unattainable and significantly enhances the therapeutic potential of SCS. Moreover, the long-term data collected by these devices can further inform personalized treatment strategies, creating a feedback loop for continuous improvement.
- Reduced Manual Adjustments: Less frequent visits for re-programming.
- Personalized Pain Relief: Adapts to individual patient needs and pain fluctuations.
- Improved Efficacy: Higher success rates in reducing chronic pain severity.
- Enhanced Patient Experience: More comfortable and less disruptive therapy.
The enhanced AI-driven SCS represents a paradigm shift from reactive to proactive pain management. By leveraging artificial intelligence, clinicians can offer a more sophisticated and effective solution to patients who previously found limited success with other treatments. This technology not only helps manage pain but also aims to improve overall functional capacity and reduce the reliance on analgesic medications, particularly opioids. The safety profile of this new SCS system is also rigorously evaluated, ensuring that these advanced capabilities do not compromise patient well-being.
2. Non-Opioid, Long-Acting Peripheral Nerve Block (PNB)
A significant breakthrough in 2025 is the FDA approval of a novel non-opioid, long-acting peripheral nerve block (PNB) specifically designed for extended pain relief following surgical procedures and for certain chronic localized pain conditions. Traditional PNBs offer temporary relief, typically lasting a few hours to a day, often necessitating supplementary opioids post-surgery. This new formulation utilizes an innovative sustained-release technology that encapsulates an anesthetic, allowing it to be slowly released over several days or even weeks. This extended duration of action can drastically reduce the need for opioid prescriptions, a critical step in combating the opioid crisis while ensuring effective pain management.
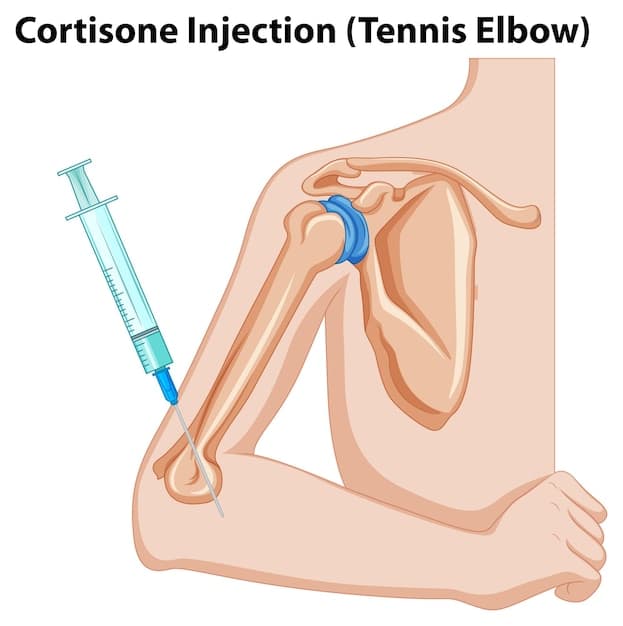
The treatment involves a single injection near the nerve responsible for transmitting pain signals to a specific area of the body. Its long-acting nature makes it an attractive option for patients undergoing major surgeries, such as joint replacements or abdominal procedures, where post-operative pain can be severe and prolonged. Furthermore, it is also being explored for its potential in managing localized chronic neuropathic pain conditions that do not respond well to oral medications. By directly targeting the peripheral nerves, systemic side effects often associated with oral pain medications are minimized, leading to a safer and more tolerable treatment experience. This innovative PNB offers a bridge between short-term acute pain management and the complex long-term needs of chronic pain patients, providing a valuable tool in the armamentarium of pain specialists.
Benefits and Applications of Long-Acting PNBs
The primary advantage of this long-acting PNB is its ability to provide sustained, localized pain relief without the systemic side effects or addictive potential of opioids. This is particularly crucial in the recovery phase after surgery, where effective pain control can significantly improve patient mobility, reduce hospital stays, and accelerate rehabilitation. The non-opioid nature also addresses concerns about patient safety and public health, offering a responsible alternative to traditional pain management protocols. For chronic pain, it represents a potential alternative to daily medication regimens, providing periods of sustained relief and improving quality of life. The treatment protocol involves careful selection of patients and precise administration by trained professionals to ensure optimal outcomes.
- Opioid Sparing: Significantly reduces or eliminates the need for post-operative opioids.
- Extended Pain Relief: Provides pain control for several days to weeks from a single shot.
- Reduced Side Effects: Localized action minimizes systemic adverse effects.
- Improved Patient Experience: Enhances recovery and functional outcomes post-surgery.
This FDA approval is a testament to the ongoing efforts to develop safer and more effective pain management strategies. The long-acting PNB offers a powerful tool for clinicians to manage both acute post-surgical pain and specific chronic localized pain conditions, significantly improving patient outcomes and contributing to a broader shift away from opioid reliance. Its targeted mechanism of action provides relief where it is most needed, for an extended duration, setting a new standard in pain intervention. The rigorous clinical trials supporting its approval confirm its efficacy and safety profile, instilling confidence in its use.
3. Vagus Nerve Stimulator (VNS) for Fibromyalgia
The third significant FDA approval in 2025 is for a novel application of Vagus Nerve Stimulation (VNS) specifically tailored for the management of fibromyalgia. Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, sleep disturbances, and cognitive dysfunction, often resistant to conventional therapies. While VNS has been approved for other conditions like epilepsy and depression, its recent expanded indication addresses the complex neurobiological underpinnings of fibromyalgia, particularly its association with autonomic nervous system dysfunction and central sensitization. This innovative VNS device works by delivering gentle electrical impulses to the vagus nerve, which plays a crucial role in regulating the body’s inflammatory response, pain perception, and mood.
The approved VNS system for fibromyalgia is non-invasive, typically applied through a device worn externally on the ear or neck, offering a less intrusive alternative to implanted devices. Patients can self-administer treatments at home, following a prescribed schedule. Clinical studies have shown that regular VNS therapy can modulate neural pathways involved in pain processing, reduce systemic inflammation, and improve sleep patterns in fibromyalgia patients. This leads to a significant reduction in pain intensity, improved physical function, and a better overall quality of life. The non-pharmacological nature of VNS is particularly appealing for patients seeking alternatives to medications that may have side effects or be ineffective. This novel application of VNS therapy provides a non-addictive and generally well-tolerated treatment option for a patient population in dire need of new therapeutic strategies.
How VNS Impacts Fibromyalgia Symptoms
Vagus nerve stimulation influences several key physiological processes that are often dysregulated in individuals with fibromyalgia. By stimulating the vagus nerve, the device helps to activate the parasympathetic nervous system, promoting a state of calm and reducing the “fight-or-flight” response often heightened in chronic pain conditions. This activation can lead to a decrease in pro-inflammatory cytokines, which are implicated in fibromyalgia pain and fatigue. Furthermore, VNS is known to modulate neurotransmitters like serotonin and norepinephrine, contributing to improvements in mood and sleep, common comorbidities of fibromyalgia. The cumulative effect is a more balanced autonomic nervous system, leading to a reduction in the widespread pain and other debilitating symptoms of the condition.
- Pain Reduction: Modulates central pain processing pathways.
- Fatigue Improvement: Influences energy levels and sleep quality.
- Mood Enhancement: Positively impacts anxiety and depression often linked to fibromyalgia.
- Non-Invasive: External device application, avoiding surgical implantation.
The FDA approval of VNS for fibromyalgia underscores a growing recognition of the role of the nervous system’s regulatory functions in chronic pain. This treatment offers a unique approach that targets multiple symptoms of fibromyalgia simultaneously, presenting a significant advance for patients who have found limited success with conventional treatments. Its non-pharmacological, non-invasive nature makes it an attractive and safe long-term option, providing a new pathway for managing this complex and challenging condition. The positive clinical outcomes highlight the potential for neuromodulatory therapies in conditions previously considered intractable.
4. Gene Therapy for Neuropathic Pain (Targeting Nav1.7 Channel)
Perhaps one of the most futuristic and potentially transformative FDA approvals in 2025 is the first-ever gene therapy specifically designed for chronic neuropathic pain, targeting the Nav1.7 sodium channel. Neuropathic pain, resulting from nerve damage, is notoriously difficult to treat, often involving severe burning, shooting, or prickling sensations. The Nav1.7 sodium channel plays a critical role in the transmission of pain signals, and genetic mutations affecting this channel have been linked to conditions ranging from congenital insensitivity to pain to inherited erythromelalgia. This innovative gene therapy aims to silence or downregulate the expression of the Nav1.7 channel in affected nerve cells, thereby reducing the hyperexcitability that contributes to neuropathic pain.
The therapy involves delivering a modified viral vector, typically an adeno-associated virus (AAV), containing genetic material that interferes with Nav1.7 production. This vector is administered via a localized injection, ensuring that the therapeutic effect is concentrated in the area of pain, minimizing systemic exposure. Early clinical trials demonstrated remarkable success, with a significant reduction in pain intensity and an improvement in neurological function in patients with severe, intractable neuropathic pain conditions, such as post-herpetic neuralgia and painful diabetic neuropathy. This approach represents a true paradigm shift, moving beyond symptomatic relief to address the fundamental biological mechanisms of pain at a genetic level. The potential for long-lasting relief from a single treatment could revolutionize the lives of many chronic pain sufferers. This form of precision medicine exemplifies the cutting edge of biotechnological advancements in pain management.
The Promise of Genetic Intervention for Pain
Gene therapy for pain management opens up entirely new avenues for treatment. By directly manipulating gene expression, clinicians can target specific pain pathways with unprecedented precision. The Nav1.7 channel has been a focus of pain research for years due to its central role in pain signaling. Silencing this channel offers the potential for profound and selective pain relief without affecting other vital physiological functions. This approach bypasses many of the challenges associated with traditional pharmacotherapy, such as off-target side effects and the need for continuous medication. The aim is to provide a durable therapeutic effect, potentially offering years of relief from a single treatment, which would be a monumental achievement in pain medicine. The long-term safety and efficacy are still under meticulous observation, but initial results are highly encouraging.
- Targeted Relief: Specifically addresses the genetic basis of neuropathic pain.
- Long-Lasting Effect: Potential for durable pain relief from a single treatment.
- Reduced Side Effects: Localized administration minimizes systemic impact.
- Revolutionary Approach: Addresses pain at its genetic and molecular root.
The FDA’s approval of a gene therapy for neuropathic pain is a landmark event, signifying the maturation of gene editing technologies for chronic disease management. While still in its early stages of widespread adoption, this treatment offers immense promise for individuals suffering from conditions that have historically been resistant to treatment. It embodies the future of precision medicine in pain, where therapies are tailored not just to the individual, but to their specific genetic predispositions to pain. This high-level intervention paves the way for further research into genetic targets for other forms of chronic pain, opening up a new frontier in therapeutic development.
5. Wearable Biofeedback System for Migraine Prevention
The fifth significant FDA approval in 2025 focuses on a wearable biofeedback system designed for migraine prevention. Migraine is a debilitating neurological condition affecting millions, and while acute treatments exist, preventing attacks remains a clinical challenge. This innovative system combines advanced sensor technology with real-time biofeedback and personalized coaching, empowering patients to proactively manage their migraine triggers and physiological responses. The device, typically worn on the wrist or head, continuously monitors physiological parameters such as heart rate variability, skin temperature, and muscle tension, which are often indicative of impending migraine attacks or stress levels contributing to them.
When the system detects physiological profiles associated with increased migraine risk, it provides immediate feedback to the user through gentle vibrations, auditory cues, or a connected smartphone app. This feedback trains patients to consciously alter their physiological state—for example, by practicing relaxation techniques or deep breathing exercises—thereby preventing a migraine from fully developing or reducing its severity. Studies have showcased its effectiveness in reducing both the frequency and intensity of migraine attacks, particularly for individuals with episodic and chronic migraines who prefer non-pharmacological interventions. This proactive, patient-centric approach offers a new layer of control over a condition that often feels unpredictable, significantly improving quality of life for sufferers. The device’s ease of use and ability to provide continuous monitoring outside of a clinical setting make it a powerful tool for self-management.

Empowering Patients Through Biofeedback
Biofeedback therapy, while not new, has historically required in-clinic sessions with specialized equipment. This wearable system democratizes access to effective biofeedback, bringing it directly to the patient’s daily life. The real-time monitoring and immediate feedback loop allow individuals to develop a stronger mind-body connection, learning to recognize and mitigate their unique physiological responses to stress and migraine triggers. The personalized coaching provided through the companion app further enhances its efficacy, offering guided exercises and insights based on the user’s data. This combination of technology and behavioral therapy provides a sustainable and empowering solution for migraine prevention, reducing reliance on abortive medications and improving overall migraine management. The emphasis is on teaching patients self-regulation techniques that can be applied in various situations.
- Proactive Prevention: Helps avert migraines before they fully develop.
- Personalized Coaching: Tailored guidance based on individual physiological data.
- Non-Pharmacological: Offers an alternative or complement to medication.
- Enhanced Self-Management: Empowers patients with real-time feedback and control.
The FDA approval of this wearable biofeedback system for migraine prevention marks a significant step towards integrated, holistic pain management. It leverages technological innovation to provide a non-invasive, user-friendly tool that addresses the multifactorial nature of migraines. By empowering patients to take an active role in their health management, this device offers a promising avenue for reducing the burden of migraine disease and improving daily functioning without the risks associated with long-term medication use. It represents a shift towards digital therapeutics that offer personalized, evidence-based interventions for chronic conditions, providing a new dimension of care.
| Key Treatment | Brief Description |
|---|---|
| 🎯 Targeted SCS with AI | AI-driven spinal cord stimulation for precise, personalized chronic pain relief. |
| 💉 Long-Acting PNB | Non-opioid peripheral nerve block offering extended post-surgical and localized chronic pain relief. |
| 👂 VNS for Fibromyalgia | Non-invasive vagus nerve stimulation system for managing fibromyalgia symptoms. |
| 🧬 Gene Therapy for Neuropathic Pain | First-ever gene therapy targeting Nav1.7 channel for long-lasting neuropathic pain relief. |
Frequently Asked Questions About New Chronic Pain Treatments
While these treatments have received FDA approval in 2025, their widespread availability may vary. Initial rollout often prioritizes specialized pain clinics and academic medical centers. Insurance coverage and provider training will also influence their broader accessibility. Patients should consult with their healthcare providers to determine if these options are suitable and available in their region.
Many of these new therapies, particularly the non-opioid peripheral nerve block and VNS for fibromyalgia, are specifically designed to reduce or eliminate the need for opioid medications. The AI-driven SCS also aims to improve pain control with less reliance on pharmaceuticals. While not universally replacing all medications, they offer strong alternatives and complements to minimize opioid use.
Side effects vary by treatment. Targeted SCS carries surgical risks like infection or lead migration, though AI-enhancements reduce programming issues. Long-acting PNBs may cause temporary numbness or mild irritation at the injection site. VNS typically has minor side effects such as voice changes or throat irritation. Gene therapy, being novel, requires careful long-term monitoring, but localized administration minimizes systemic risks. Your doctor will discuss specific risks.
Eligibility depends on the specific treatment and the patient’s individual condition. Targeted SCS and long-acting PNBs are often for specific neuropathic or post-surgical pain. VNS is approved for fibromyalgia patients who haven’t responded to other therapies. Gene therapy for neuropathic pain is likely for severe, intractable cases. A thorough medical evaluation by a pain specialist is essential to determine suitability for any of these advanced options.
The onset of relief varies. Long-acting PNBs offer immediate post-procedure relief lasting weeks. SCS and VNS may require an adjustment period, with optimal benefits developing over weeks to months as the body adapts to stimulation. Gene therapy, while potentially long-lasting, might have a delayed onset as gene expression changes take effect. Your physician will set realistic expectations for each specific treatment.
Conclusion
The FDA’s approval of these five innovative treatments for chronic pain in 2025 marks a transformative period in pain management. From AI-driven neuromodulation to sophisticated gene therapies and personalized biofeedback systems, these advancements offer renewed hope for millions. They represent a significant shift toward more precise, less invasive, and non-opioid solutions, addressing the complex and diverse nature of chronic pain. As these cutting-edge therapies become more accessible, they promise not only to alleviate suffering but also to restore functionality and improve the overall quality of life for individuals grappling with persistent discomfort. This new era in pain care underscores a commitment to integrating pioneering science and technology to create a healthier, less painful future.